Michigan Pharmacy Researchers Tackle COVID-19 From Every Angle
October 15, 2020
As the world continues to struggle with the COVID-19 pandemic, most Americans have seen large shifts in their daily lives. Similarly, research, practice, and education within the University of Michigan College of Pharmacy has undergone significant changes.
Students are practicing distant learning, utilizing new technologies during in-person classes, working in the lab in shifts, and creatively building communities and staying connected. Faculty clinicians are optimizing telepharmacy, wearing more PPE, planned a field hospital, and more.
Researchers at Michigan Pharmacy quickly adapted to address issues related to the pandemic. Faculty are applying their expertise to find solutions to many of the pressing issues related to the pandemic, from developing new therapies to ensuring that patients receive their routine medications.
Drs. Steve and Anna Schwendeman are developing investigational treatments for COVID infected patients.
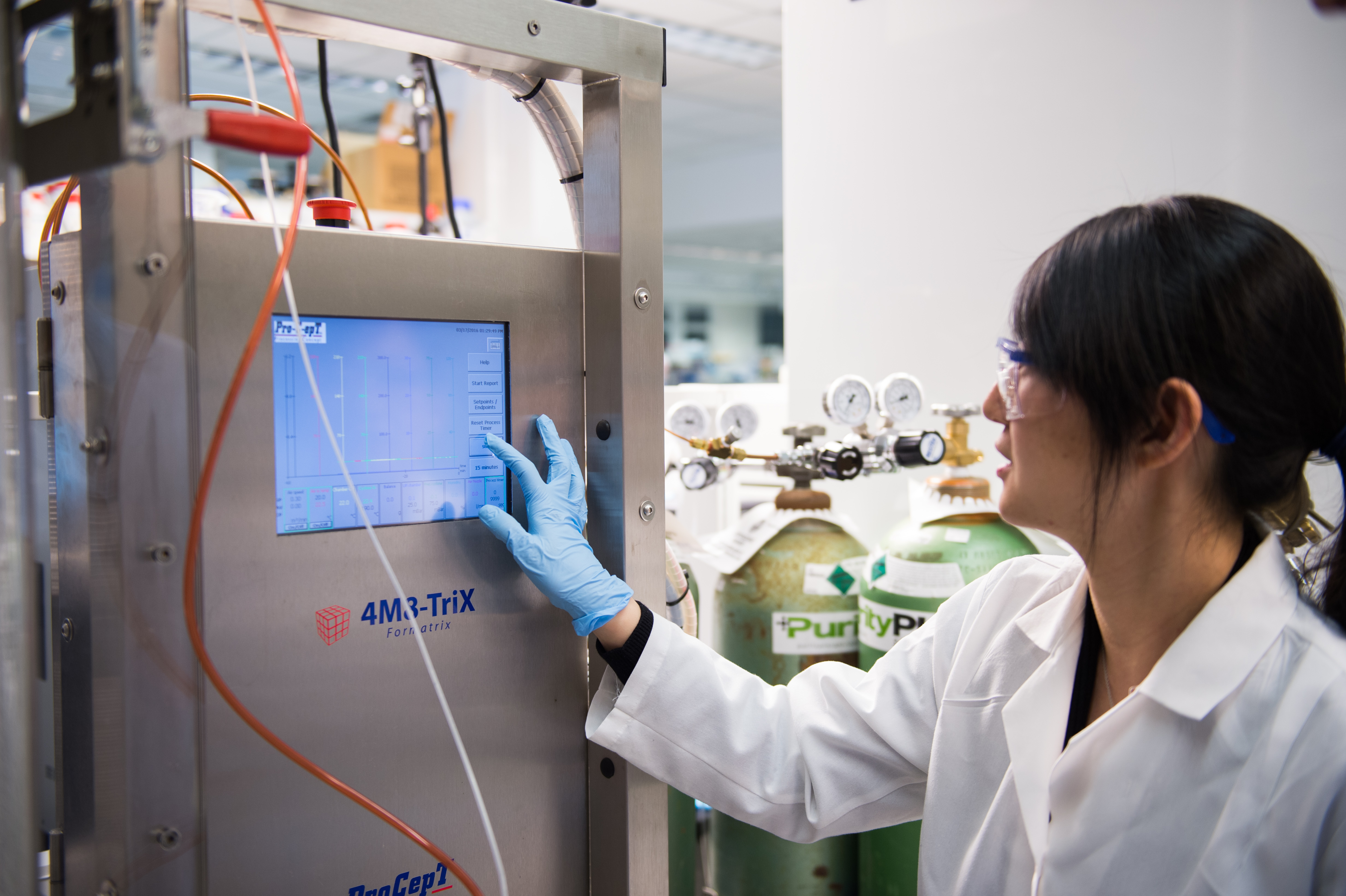
Dr. Steve Schwendeman is exploring photochemically generated nitric oxide (NO) For COVID-19 treatment. “The small gaseous radical, NO turns out to be a key molecule in combating COVID-19,” says Dr. Schwendeman. “NO is normally produced in the upper airways and serves as the first line of defense against viral and bacterial infections of the airways. Conditions associated with impaired NO production increases the risk of poor outcomes in COVID-19 and it has been demonstrated that NO inhibits the replication of coronavirus. Inhalation of gas phase NO could be useful in the prevention and treatment of COVID-19.”
However, due to its instability, gas cylinder based technologies are extremely expensive and available only in the hospital setting. “Our research team is working on innovative technologies for safe and economic, on-demand generation of inhalable NO,” says Dr. Schwendeman.
Dr. Anna Schwendeman is attempting to prevent the COVID cytokine storm by attaching drugs to synthetic high-density lipoprotein (sHDL). “In our previous research, we found that HDL cholesterol levels are low in septic patients and infusions of synthetic HDL can rescue mice from death in an animal model of sepsis,” notes Dr. Schwendeman. “The efficacy on sHDL infusions in sepsis seems to be correlated with its ability to inhibit the cytokine storm and microvascular thrombosis and reduces endothelial dysfunction. The same cardiovascular pathology and reduction of HDL cholesterol levels are seen in COVID-19 patients. Because of these points, we are exploring the ability of sHDL infusions to reverse cardiovascular pathologies associated with COVID-19.”
A group of faculty are developing strategies for optimizing existing anti-COVID therapies.
Dr. Haojie Zhu is working to identify and activate the hydrolases of remdesivir (GS-5734) and EIDD-2801 in COVID-19 patients’ lungs. “Remdesivir and EIDD-2801 are viral RNA-dependent RNA polymerase inhibitors and have shown promising anti-SARS-CoV-2 activity in vitro and in vivo,” says Dr. Zhu.
The FDA recently issued an Emergency Use Authorization allowing remdesivir to treat patients with severe COVID-19. EIDD-2801 is undergoing phase II clinical trials in COVID-19 patients. However, the clinical benefits of both medications appear to be modest, and many patients did not respond adequately to remdesivir and EIDD-2801. “Identifying factors contributing to the inter-individual variability in response to the treatment could improve therapeutic outcomes by individualizing the pharmacotherapy regimen – for example, drug selection, doses, and dosing frequency,” explains Dr. Zhu.” “This project could directly impact the therapeutic management of severe COVID-19 patients and may lead to the development of a personalized pharmacotherapy regimen to treat COVID-19.”
Dr. Tim Cernak is using artificial intelligence to find alternative pharmaceutical building blocks for 12 drugs under investigation to treat COVID-19. Researchers fear that the same issues with supply chains that caused widespread shortages at the beginning of the pandemic in the United States may result in the same problem with the fine chemicals needed to synthesize COVID-19 therapeutics and vaccines. Dr. Cernak’s work aims to insure that once we have a potent COVID-19 therapy identified, we will be able to produce it on a large enough scale.
Another group of Michigan Pharmacy faculty are exploring more effective COVID-19 treatments in clinical and community settings.
“While caring for critically ill COVID-19 patients on the ventilator, we started to notice that they developed hypertriglyceridemia, a side effect from propofol, more frequently than what we were used to for our traditional non-COVID-19 patients,” notes Dr. Michael Kenes. “We conducted a prospective, observational study and demonstrated that even though overall markers of severity of illness and degree of lung injury were similar, a third of patients with COVID-19 developed hypertriglyceridemia compared to only around 5% of non-COVID-19 patients, putting those COVID patients at a higher risk of adverse cardiac events. This is important because once a patient develops hypertriglyceridemia, propofol has to be discontinued and alternative or less preferred sedative medications have to be utilized to avoid serious complications. We also are able to utilize our findings to help guide medication use estimations for our COVID-19 ICU patients and hopefully mitigate medication shortages that many hospitals across the country experienced during the first surge.”
In a paper published in Clinical Infectious Diseases, Drs. Greg Eschenauer and Jason Pogue identified that critically ill COVID-19 patients who received a single dose of a drug that calms an overreacting immune system were 45% less likely to die overall, compared with those who did not receive the drug. Intravenous administration of tocilizumab lowered mortality despite patients having twice the risk of developing an additional infection, on top of the novel coronavirus.
In March 2020, Dr. Sarah Vordenberg collaborated on a survey of over 1,400 adults aged 65 years and older across the United States to explore how they planned to obtain medication refills at the beginning of the COVID-19 pandemic. Obtaining medications posed a potentially difficult tradeoff for older adults – go to the pharmacy and risk exposure to the virus, have someone else deliver the medication and increase that person’s risk, or decrease or stop their medication and risk worsening health. Most participants reported health conditions such as heart disease or diabetes that would increase their risk of serious illness from COVID-19.
“More than half of participants indicated that they planned to keep going to the pharmacy to get refills as they normally would, even if they had multiple chronic health conditions,” says Dr. Vordenberg. “This work led to an article in The Conversation to increase awareness of strategies for older adults to safely obtain medications.”
Researchers are looking at the pandemic from another angle: preventing it in the first place. Drs. James Moon and Wei Cheng are working on separate projects addressing vaccine development.
Dr. Wei Cheng and his laboratory have developed a platform technology that can produce complete synthetic particles that both qualitatively and quantitatively mimic the essential biological features of enveloped viruses. Using this technology, Dr. Cheng and collaborators are investigating how the virus that caused COVID-19 may induce either harmful or protective immune responses and to utilize this knowledge for the development of the next-generation antiviral vaccines.
“SARS-CoV-2, the virus that causes COVID-19, enters host cells via the interaction between Receptor Binding Domain (RBD) of viral spike protein (S-protein) and host cell’s angiotensin-converting enzyme 2 (ACE2) expressed by human alveolar epithelial cells,” explains Dr. James Moon. “N-protein is the most abundant protein of SARS-CoV-2, serving as a structural protein required for viral assembly and shedding. Hence, N-protein, S-protein, and RBD are promising targets for generating T-cell and antibody responses against SARS-CoV-2. However, current protein-based vaccine delivery systems generate weak concerted T-cell and antibody responses.”
To address these challenges, the Moon laboratory is developing a new nano-vaccine system for stable lymph node targeted delivery of SARS-CoV-2 antigens and induction of T-cell and Ab responses against SARS-CoV-2. The Moon lab has previously shown that mice immunized with this nano-vaccine system can elicit potent immune responses against Ebola viral infection. Based on this technology, Dr. Moon aims to apply this vaccine platform for rapid development of a COVID-19 vaccine.
COVID-19 continues to affect every element of our lives, and a solution to the pandemic will need to be multi-dimensional. The University of Michigan College of Pharmacy’s faculty are hard at work addressing many elements of the disease, hopefully getting us one step closer to normalcy.
Latest News
Professor Amanda Garner Named Charles Walgreen, Jr. Professor
March 28, 2025
Author: Markie Heideman, Content Marketing Manager Media Contact: Lindsay Groth, Director of Marketing and Communications, [email protected] Amanda Garner, PhD, has been named Charles Walgreen, Jr. Professor of Medicinal Chemistry, as approved by the Regents of the University of Michigan. Both The Charles Walgreen, Jr. Professorship created in December 2024 and the already-established Charles R. Walgreen, […]
Professor Shiyanbola Elected to Behavioral Medicine Fellowship
March 27, 2025
This SBM fellowship is not only a recognition of Dr. Shiyanbola’s hard work but an opportunity to mentor early-career investigators.
Dr. Hanna Phan Selected for Excellence Award in Pediatric Pharmacy Practice
March 21, 2025
Dr. Phan’s dedication to improving pediatric health outcomes, particularly in pulmonology, and her passion for mentorship and education have earned her this prestigious honor.
