Professor Kathleen Stringer Searches for the Signals of and Treatments for Sepsis
January 6, 2025
By: Toni Shears
 Each year, at least 1.7 million adults in America develop sepsis.* At least 20 percent of adults with this extreme, life-threatening response to infection die in the hospital or enter hospice. Sepsis is involved in one out of every three patient deaths in the hospital.
Each year, at least 1.7 million adults in America develop sepsis.* At least 20 percent of adults with this extreme, life-threatening response to infection die in the hospital or enter hospice. Sepsis is involved in one out of every three patient deaths in the hospital.
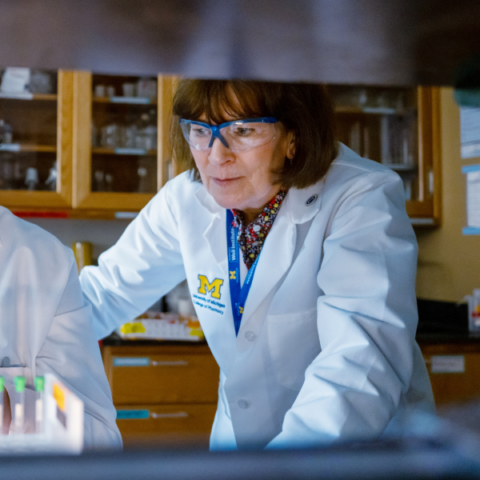
Yet once an infection turns into sepsis and triggers an organ-damaging chain reaction throughout the body, we have no effective drugs to treat it. This is where Kathleen Stringer, PharmD, Albert B. Prescott Collegiate Professor of Clinical and Translational Pharmacy, focuses her research. She sifts through the metabolites spun off within cells during sepsis, looking for biomarkers that may be potential targets for drug candidates.
“To identify drug candidates, you have to understand the mechanism behind the disease so you can target the biochemistry involved. That’s always been my philosophy,” says Dr. Stringer. She relies on metabolomics —the systematic study of the small molecules that cellular processes leave behind in the blood— to understand the physiology playing out in critical disease states like sepsis and acute respiratory distress syndrome (ARDS).
Small molecules like lactate, cholesterol and creatinine can signal disease and measuring them is the diagnostic cornerstone of clinical medicine. We have no such signal we can test for in acute, critical illness, Stringer points out. Also, sepsis is a syndrome – a cluster of common symptoms like fever and accelerated heart rate that could be signs of other conditions.
“Sepsis is not like cancer. In my field, we have oncology envy because cancer involves a well-defined pathology. We don’t have that in critical illness like sepsis,” she says. “So, one of the things that we’re trying to do is identify the key features and markers that we need to measure in that acute setting. This could direct the development of l point-of-care tests, but we’re not quite there yet.”
Professor Kathleen Stringer Searches for the Signals of and Treatments for Sepsis
Metabolomics lends itself very well to this effort because it analyzes the final phases of a cascade of cellular and biochemical processes, from the individual genes (genomics) to mRNA transcription and proteins produced (proteomics) to the metabolome — the end product of cellular activity.
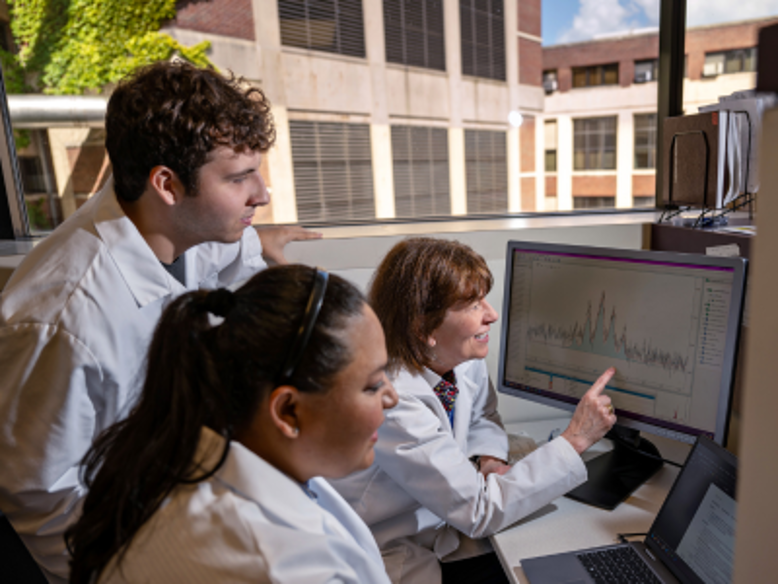
Sepsis plays out differently across patients. With her lab team, Stringer, who is also a Professor of Internal Medicine at Michigan Medicine, is trying to figure out if there are patterns and genetic differences in how they interact. “Are there groups of patients with certain types of signals that we could put in one bucket and different signals that we could put in another bucket?” she wonders. This has been demonstrated in a number of studies so it does appear that there are different sepsis phenotypes.
“One way to find out is to phenotype patients,” says Stringer, “There may be a genetic predisposition to certain metabolic signals that we see in sepsis that could help us phenotype or endotype sepsis patients. If we can categorize these patients on a more granular pathologic and physiologic level, that could help us identify targets for drugs that can treat those types of patients,” she notes. She is pursuing a grant to study genetically linked metabolites in sepsis.
Typically, organ failure is the ultimate cause of death in sepsis, and no organ is spared, but some organs may weather the infectious storm better than others. “We’re trying to figure out why,” Dr. Stringer says. In studying models of sepsis and different organ responses and their metabolic consequences, “We can see over time that the metabolic profile of the liver is very different from the metabolic profile of the kidney. Understanding these changes in physiology and how sepsis influences them could help us better identify blood markers that might indicate what is happening at the organ level during sepsis. These could be points for therapeutic intervention.”
Historically, clinical trials of studies have a poor track record. This makes enriched enrollment of sepsis patients using specific biomarkers important. She is also working with her close collaborator, Dr. Robert Dickson, Associate Professor of Internal Medicine, and the Galen B. Toews Legacy Professor of Pulmonary and Critical Care Medicine, to understand the contribution of the gut microbiome since it has a metabolome of its own. It is often difficult to parse out metabolites generated by gut microbes that are specific or related signals of disease.
Stringer’s ultimate goal is to use metabolites to pinpoint the molecules and processes involved in sepsis and ARDS so researchers can identify and test existing drugs or develop new ones to interrupt the pathology. Her work on the leading edge of drug discovery may give us new approaches to halt common critical illnesses that have, until now, eluded treatment.
* Rhee C, Dantes R, Epstein L, Murphy DJ, Seymour CW, Iwashyna TJ, Kadri SS, Angus DC, Danner RL, Fiore AE, Jernigan JA, Martin GS, Septimus E, Warren DK, Karcz A, Chan C, Menchaca JT, Wang R, Gruber S, Klompas M; CDC Prevention Epicenter Program. Incidence and Trends of Sepsis in US Hospitals Using Clinical vs Claims Data, 2009-2014. JAMA. 2017 Oct 3;318(13):1241-1249. doi: 10.1001/jama.2017.13836. PMID: 28903154; PMCID: PMC5710396.
Most Recent Stories
Building Specialized Pharmacy Services from the Ground Up
March 28, 2025
“I never dreaded getting up and going to work. I loved what I did. When things changed, I looked at it as an opportunity or a challenge.”
Bringing Pharmacy Expertise to Oncology Clinics
March 17, 2025
It was the interpersonal connection and an interest in the ever-changing landscape of oncology that piqued Dr. Hough’s interest.
PharmD Alum Takes Medication Expertise to the Boardroom
February 27, 2025
His ability to understand each new pharmaceutical is a skill he developed during his time in U-M’s PharmD program – where the curriculum focuses on problem-solving, critical thinking, leadership, research and the utilization of skills to practice as a pharmacist in any setting.